Test, Link, Call: a simple premise with a powerful purpose
In 2021, the Foundation invested in a unique idea — Test, Link, Call, an innovative proof of concept project led by Dr Sofia Bartlett, the Interim Scientific Director Clinical Prevention Services at BCCDC.
Dr Bartlett had an idea about how to better support access to care and treatment for people with HCV who experience criminalization in BC, after speaking with healthcare providers working in BC Provincial Correctional Centres who told her how difficult it was for people living with HCV to connect to treatment after they are released. Many of these people experience inequities in accessing care due to systemic and structural barriers and social determinants of health, such as poverty, gender, and Indigeneity.
“HCV is 20x more prevalent among people who are incarcerated than in the overall population in BC. However, only 41% of people who tested HCV RNA positive received curative treatment while in custody in 2021.” – Dr Sofia Bartlett
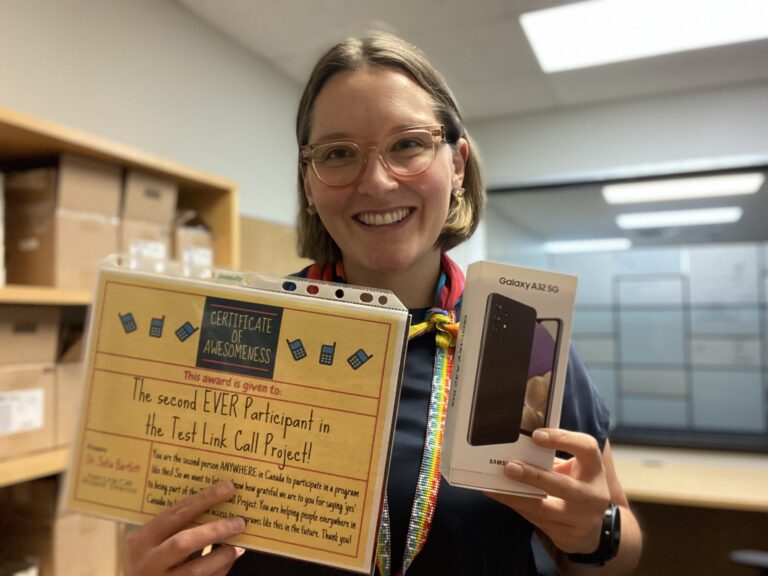
Engaging with this population is difficult, as they rarely have a cell phone or stable contact details, which means that a phone is a key tool, and a huge barrier, to accessing healthcare services. Dr Bartlett thought, “What if we gave everyone leaving custody who is living with hepatitis C a cell phone and pay their phone bill for six months?”
Initially the healthcare providers she proposed this to were skeptical, but Dr Bartlett consulted Peer Navigators who were enormously enthusiastic about the idea. From there, Test, Link, Call was born with a primary objective of improving HCV treatment uptake among this population, and to help with successful community re-integration. The premise of the original pilot was very simple — provide cell phones and peer support to people living with HCV as they are leaving BC Provincial Corrections Centres.
Test, Link, Call’s immediate success demonstrated an 81% treatment uptake, which is twice higher than what is usually achieved in this population.
Due to this immediate success and thanks to donor funding, the pilot quickly expanded to include people living in communities across the province who are at risk for HCV and also experience criminalization and other barriers in accessing the care and treatment they need.
In 2023, Test, Link, Call was expanded even further to support people who are at risk for other strains of hepatitis and additional blood-borne diseases including the human immunodeficiency virus (HIV).
Due to the overwhelming response to the program, a waitlist was created in the summer of 2023 and the team introduced new cohorts of 50 spots as soon as funding becomes available. Amazing momentum is being achieved with new enrollments on average of 22 people per month as of September 2023.
Test, Link, Call is an important strategy to support our province’s progress towards achieving the World Health Organization and Canada’s goal of eliminating HCV, HBV, and HIV, which present an increasing burden on the healthcare system as affected populations age.
Key to achieving this goal is identification of population groups that are disproportionately affected by all of these diseases. This includes people who experience criminalization such as individuals who are incarcerated, use drugs, are unstably housed, or experiencing other barriers to accessing healthcare services due to systemic issues, such as stigma and discrimination.
The program also promotes additional wrap-around services and support such as culturally-safe apps designed for Indigenous health and wellness, and support for substance use. During the first year of the program, two accidental overdoses were attended by First Responders after participants used these apps.
With generous donor funding and collaboration, Test, Link, Call has increased the uptake of dedicated care and treatment for the populations served. As of World Hepatitis Day in July 2023, the program had connected 200 people to HCV care, which equates to at least 60 liver-related hospitalizations that have been prevented, and at least two deaths from liver cancer or liver failure averted.
With treatment costs in excess of $20,000 per person for liver-related hospitalizations and nearly $95,000 for liver cancer treatment per person, it’s clear that the Test, Link, Call program has a significant cost-benefit at a comparative cost of approximately $1,000 per person enrolled in the program.
Test, Link, Call’s success to date has proven it has the potential to change the current trajectory of these diseases and begin to reverse years of chronic under investment. It’s a great example of proactive and compassionate public health that meets people’s needs, in their community.
Your support for this project will help to increase equitable access to care and treatment for people at risk of these diseases due to many social determinants of health, along with elevating a sense of value for the individuals participating in this innovative program.
The Foundation is committed to helping to create a more inclusive and just society by addressing the unique needs and challenges faced by specific populations who experience systemic disadvantages, discrimination, or unequal access to opportunities and resources, such as people who are incarcerated and people who use drugs.



